Scientists at the Jagiellonian University in Kraków have uncovered a groundbreaking discovery that could significantly improve the outcomes of bone marrow transplants, a key treatment for blood cancers such as leukemia and lymphoma.
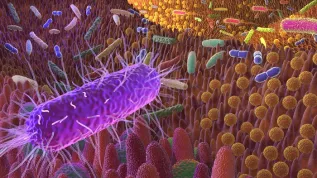
Their research has shown that endothelial cells, which line blood vessels, play a critical role in the regeneration of the bone marrow niche after transplant procedures, challenging previous beliefs about the role of stem cells in this process.
The study, published in the journal Cell Reports (https://doi.org/10.1016/j.celrep.2024.114779) reveals that differentiated endothelial cells—which were thought to be limited in regenerative capacity—can actually re-enter the cell cycle and rebuild blood vessels in response to stress. This discovery undermines the long-held assumption that rare stem cells are primarily responsible for regenerating the marrow niche after conditioning, a process that involves chemotherapy or radiation to prepare a patient for a transplant.
Endothelial Cells Are Key to Recovery
The bone marrow niche, a specialized microenvironment crucial for the proper functioning of hematopoietic stem cells (HSCs), is vital for the success of bone marrow transplants. However, the aggressive conditioning process, which is essential for transplant success, also damages the endothelial niche. As many as 40% of endothelial cells can die within the first two months after transplantation, making niche regeneration a critical factor in recovery.
'The niche is a specialized microenvironment in the bone marrow, necessary for the proper functioning of haematopoietic stem cells. In order for the transplanted cells to be accepted and to perform their function, the recipient's marrow niche must regenerate quickly after the conditioning process is completed. Our study concerned the mechanisms behind this regeneration and the role of endothelial cells, which build the inner lining of blood vessels', Krzysztof Szade, PhD, from the Faculty of Biochemistry, Biophysics and Biotechnology at Jagiellonian University, said.
Previous theories suggested that a rare population of specialized stem cells was responsible for regenerating the endothelial layer. However, the researchers from Jagiellonian University used advanced single-cell RNA sequencing (scRNA-seq) and rainbow mice—genetically modified animals that allow scientists to track cell divisions through fluorescent proteins—to identify the true source of this regeneration.
Their findings were groundbreaking: as many as 25% of differentiated endothelial cells were able to divide and regenerate blood vessels, showing remarkable plasticity under stress. This discovery has the potential to reshape future strategies for improving recovery following bone marrow transplants.
'We performed an analysis of gene expression at the single-cell level. First, we isolated these cells from the mice, determined the expression of all genes in each of them, and finally - among the different types of cells - we found those that could potentially be stem cells. And that was our first suspicion: that there were some precursor cells from which all regeneration would start’, Szade said.
Mathematical Model for Regeneration
In addition to their biological findings, the research team developed a mathematical model using graph theory and neural networks to simulate the processes of endothelial regeneration. This model, developed by former biotechnology student Jan Morys, quantitatively demonstrated how endothelial cells contribute to vessel repair, providing a new tool for understanding the dynamics of bone marrow niche regeneration.
Szade said: ‘Our study shows that endothelial cells exhibit much more plasticity than previously thought. They can adapt and contribute to blood vessel repair in stressful conditions, which opens up new possibilities for improving transplant outcomes."
Implications for Bone Marrow Transplantation
This new understanding of endothelial regeneration could have far-reaching implications for bone marrow transplantation, especially in patients undergoing the demanding conditioning process. By focusing on enhancing the regenerative capacity of endothelial cells, researchers believe it may be possible to reduce transplant complications and accelerate recovery, ultimately improving the quality of life for patients.
Moreover, this discovery could be applied to a variety of conditions beyond blood cancers, including genetic and immunological diseases, where bone marrow transplantation is increasingly used.
Szade added: ‘Understanding how endothelial cells regenerate the marrow niche is the first step in improving bone marrow transplantation for a range of diseases. We can now explore therapies that could help boost endothelial plasticity, making the process of recovery faster and more efficient.’
A New Era in Regenerative Medicine
The study from Jagiellonian University marks an important milestone in the field of regenerative medicine, with potential applications extending far beyond bone marrow transplants. By rethinking how the body heals itself at the vascular level, the research opens doors to new therapeutic avenues that could improve the outcomes of various transplant procedures and aid in the recovery of patients facing serious diseases.
'Based on these discoveries, bone marrow transplantation could be improved so that the patient regenerates better after conditioning. Knowing the mechanisms behind this phenomenon, we could try to +boost+ the aforementioned plasticity and make the regeneration of recipients even more effective, and lower the risk of complications', Szade said.
PAP - Science in Poland, Katarzyna Czechowicz
kap/ agt/