A Polish scientist is spearheading innovative research into the treatment of peritoneal cancers, which often arise from metastases originating in the ovaries, colon, or stomach.
The cancers present unique clinical challenges, primarily due to the blood-peritoneal barrier that limits the effective delivery of chemotherapeutic agents to the peritoneal cavity, and the molecular complexity of peritoneal tumors that complicates traditional treatment strategies.
Peritoneal cancers are especially difficult to treat because conventional systemic chemotherapy is often ineffective. The blood-peritoneal barrier, a physiological feature that separates the peritoneal cavity from the bloodstream, prevents chemotherapeutic drugs from reaching therapeutic concentrations within the abdominal cavity. Furthermore, peritoneal cancers frequently reach advanced stages where surgical removal of tumors is no longer possible, necessitating the development of alternative therapeutic strategies that can deliver drugs directly to the site of the disease.
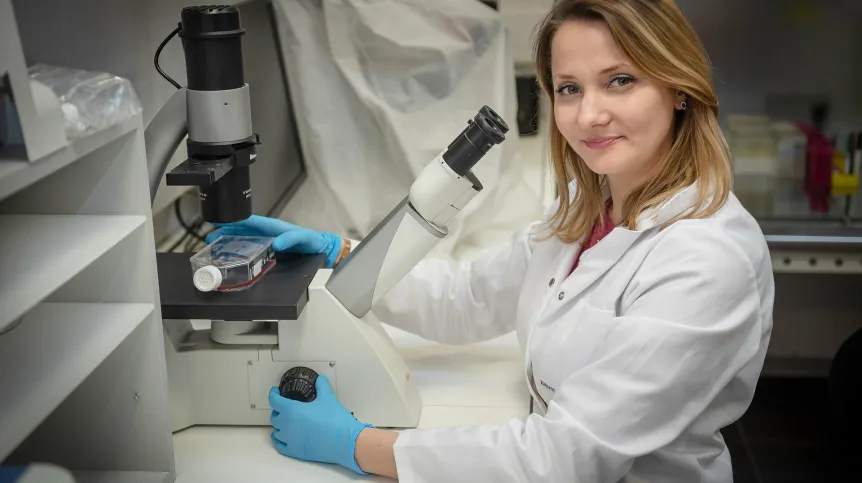
Professor Agata Mikołajczyk-Martinez from the Wrocław University of Environmental and Life Sciences who is behind the new research said: "Unlike primary cancers, peritoneal cancers typically result from metastatic spread, complicating treatment and requiring advanced technologies that can address the unique characteristics of these tumors.
"Systemic chemotherapy is largely ineffective because the drugs fail to reach the peritoneal cavity in sufficient concentrations. This challenge underscores the importance of exploring novel therapeutic approaches."
In response to these challenges, Professor Mikołajczyk-Martinez and her team are investigating a novel therapeutic approach that combines hyperthermia (controlled heating) with gas dehydration to enhance the permeability of cancerous cells, thus improving the effectiveness of chemotherapy. Preliminary in vitro studies have shown that exposing cancer cells to brief periods of heat and dehydration results in increased drug permeability, allowing chemotherapeutic agents to penetrate the tumor more effectively.
The underlying principle of this combined therapy is that dehydration and hyperthermia temporarily alter the cellular membrane properties, increasing their permeability and making it easier for therapeutic agents to enter the cells. This method not only enhances drug uptake but also minimizes the collateral damage to healthy tissues, a significant limitation of traditional chemotherapy treatments.
In addition to hyperthermia and dehydration, the research team is exploring the use of liposomes—small lipid-based vesicles that can encapsulate drugs. When administered as an aerosol and activated by ultrasound at specific locations within the body, liposomes can be targeted to release their contents precisely where needed, thereby improving the localization of drug delivery. This technique reduces the systemic side effects of chemotherapy by limiting drug exposure to non-targeted tissues.
According to Professor Mikołajczyk-Martinez: "By activating liposomes with ultrasound, we can enhance the localized delivery of chemotherapy, ensuring that the drug reaches the tumor site directly, while minimizing damage to surrounding healthy tissues." This approach represents a significant advancement in targeted drug delivery, offering the potential to improve treatment efficacy and patient outcomes.
Encouraged by the initial results, Professor Mikołajczyk-Martinez has secured funding through the LIDER XIII program, managed by the National Centre for Research and Development (NCBiR), to further develop this therapy. The research team is now working on creating a prototype device capable of delivering the combined hyperthermia and dehydration treatment in animal models. The goal is to evaluate the safety and efficacy of the approach in vivo, with the ultimate aim of translating these findings into clinical applications.
Professor Mikołajczyk-Martinez said: "Our goal is to develop a therapeutic strategy that not only prolongs survival for patients with peritoneal cancers but also provides a real opportunity for recovery. If successful, this approach could provide a much-needed alternative to current treatments, improving both the quality of life and survival rates for patients."
(PAP)
PAP - Science in Poland
ros/ agt/ kap/
tr. RL