Microbiome analysis is becoming an increasingly popular service in Poland, but experts warn that many commercial tests promise more than they can deliver, limiting their usefulness for patients, according to Paweł Łabaj from the Małopolska Centre of Biotechnology at the Jagiellonian University.
“The marketing hype surrounding the microbiome can lead patients to make poor decisions,” the expert said.
The label “microbiome testing” encompasses methods with widely varying capabilities—from simple tests for a few pathogens to advanced DNA analyses covering hundreds of species and strains. Their diagnostic value differs dramatically, but this is not always explained in commercial offers, Łabaj said.
“There are several methods on the market, each with its advantages and limitations. However, marketing communications rarely explicitly mention the latter,” he explained. The choice of method determines whether a test detects only a few pathogens or presents the full structure of the microbiome, but patients are often unaware of this.
The oldest and simplest microbiology tool is culture, in which a sample is applied to a medium and bacteria are observed after incubation. This method reveals only a fraction of intestinal microorganisms, effectively detecting selected pathogens but not describing the entire microbiome.
A newer approach involves molecular methods, including widely used PCR tests, which check for DNA of specific bacteria. “A PCR test is an excellent diagnostic tool when a physician wants to exclude the presence of specific microorganisms, but it is not suitable for describing the full composition of the microbiome,” Łabaj said. PCR tests can produce false negatives if DNA fragments mutate or false positives if a new organism shares identical sequences due to horizontal gene transfer.
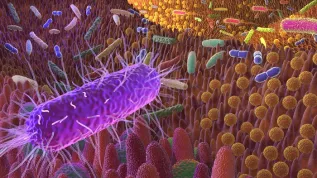
High-throughput sequencing methods, also called next-generation sequencing (NGS), were a breakthrough in microbiome research. This includes sequencing of the bacterial 16S rRNA gene, a molecular marker. Short-read sequencing of gene fragments was initially common, limiting precision. Today, long-read technologies allow analysis of the entire gene in a single run, improving bacterial distinction and providing a more accurate microbiome profile without dramatically increasing costs.
Full metagenome sequencing, covering the entire set of genomes in a sample, is even more detailed. “Full metagenome sequencing allows to identify individual bacteria, down to the strain level, which is crucial because only then can important functional differences between microorganisms become apparent,” Łabaj said.
However, full metagenome sequencing is complex and expensive. Consumer tests often reduce sequencing depth to lower costs, limiting resolution and reliability. “And interpretation is extremely important. A complete blood count (CBC) yields dozens of parameters; a microbiome test yields thousands. However, as with CBC, a single value usually means nothing if the others are within the normal range,” Łabaj explained.
Understanding results requires expert knowledge, as the balance between species is crucial. Until recently, metagenomic interpretation was not part of medical training. “Until now, metagenomic interpretation of microbiome characterization has not been included in the medical training curriculum, which is why the results of such studies sometimes fall on deaf ears. This is only now beginning to change,” Łabaj said.
Recent research indicates microbiome testing is already clinically relevant. Publications in The Lancet and Nature summarize principles and clinical trials, showing microbiome analysis can guide diagnosis and treatment.
In cases with specific pathogens, therapy decisions are straightforward and may rely on simpler tests. In more complex situations involving microbiome imbalance, comprehensive analysis enables targeted interventions like diet, supplementation, or probiotics under professional guidance. Severe, recurrent infections, such as Clostridioides difficile, may require gut microbiota transplantation, already recommended in Poland.
Łabaj cautions against self-treatment. “Even taking probiotics without consulting a specialist is not a good idea. The composition of the microbiome varies greatly geographically and across populations, so preparations that make sense in one group may be unnecessary or even harmful in another,” he said.
For example, in the Polish population, a deficiency of Bifidobacterium bacteria is often observed, while Lactobacillus is not a problem. Meanwhile, many products available in pharmacies contain both of these bacteria. Many other advertised probiotics also contain mixtures of several or a dozen strains. This is not always an optimal solution—sometimes these strains compete with each other in the intestines, which can reduce the chance of successful colonization. Therefore, consultation with a specialist, such as a dietitian, is recommended.
Lifestyle factors also influence microbiome function. “Irregular sleep, high stress levels, and insufficient fibre intake are the main factors that disrupt the microbiome. Even travelling between time zones can cause short-term intestinal problems, because the microbiome reacts to disruptions in circadian rhythms more quickly than one might think,” Łabaj said.
The scientist concluded that microbiome-based research and therapies are the future of personalized medicine, but proper diagnostics and clear communication are essential. “Unfortunately, in today's world, imprecise messages break through easily and reach a wide audience, causing people to take actions without a solid scientific basis,” he said.
Katarzyna Czechowicz (PAP)
kap/ agt/
tr. RL